Hemorrhoid Embolization
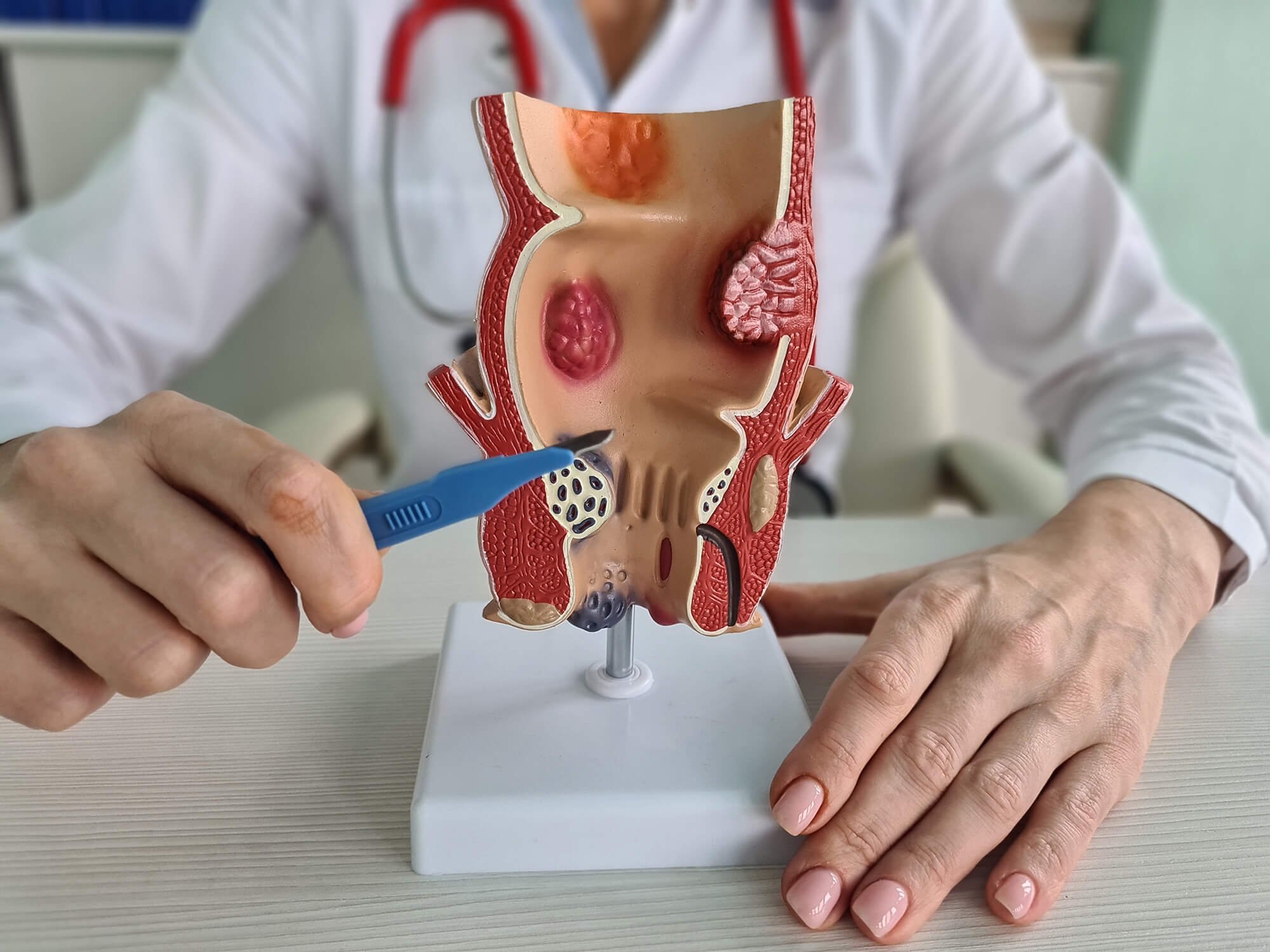
What is hemorrhoid embolization?
Hemorrhoid embolization is a minimally invasive procedure that treats hemorrhoids. When compared to surgery, recovery is much faster and you can often go home the same day.
How it works: Particles block the blood vessels supplying your hemorrhoids, causing them to shrink and disappear.
Who can get hemorrhoid embolization?
Hemorrhoid embolization treatment is generally suitable for patients suffering from symptomatic hemorrhoids who have not responded to conservative treatments such as dietary and lifestyle changes or over-the-counter medications.
It can also be an appropriate alternative for those who cannot undergo traditional surgical procedures due to reasons such as advanced age or underlying health conditions. However, every case is unique and depends on an individual's health status and the severity of hemorrhoids. Therefore, a thorough consultation with a healthcare provider is crucial to determine the suitability of hemorrhoid embolization for each patient.
How is the procedure performed?
Hemorrhoid embolization is performed by an interventional radiologist using fluoroscopic guidance. The procedure typically lasts approximately 30-45 minutes and patients can usually go home the same day.
Numbing the area:
Initially, a local anesthetic is administered to numb the area.
Injecting the particles:
Once positioned correctly, the radiologist injects small particles or coils into the hemorrhoidal arteries, effectively blocking the blood supply.
Small incision:
A small needle is then inserted into the artery through a tiny incision in the wrist or groin so a catheter can be inserted.
Hemorrhoids shrinking:
This causes the hemorrhoids to shrink and eventually disappear.
Inserting the catheter:
Using real-time imaging, the radiologist guides a catheter through the artery until it reaches the hemorrhoidal arteries.
Hemorrhoid embolization side effects
Hemorrhoid embolization, like all medical procedures, can have potential side effects.
These side effects are usually minor and temporary.
Common side effects may include discomfort, mild anal discharge, or temporary rectal bleeding.
In rare cases, complications such as infection, blood clots, or allergic reactions may occur.
It's important to note that hemorrhoid embolization is generally considered safe and less invasive compared to traditional surgical procedures for hemorrhoids.
Any concerns or symptoms should be reported to your healthcare provider for evaluation and management.
What to Expect During a Visit?
During your visit to the healthcare provider for hemorrhoids, you can expect a detailed discussion about your symptoms, medical history, and lifestyle habits.
The next step is the physical examination, which may involve a visual inspection of your anal area and a digital rectal examination. Depending on your symptoms and the findings of the preliminary examination, further diagnostic tests like an anoscopy, sigmoidoscopy, or colonoscopy may be recommended.
Your provider will then discuss the appropriate treatment options, which may range from lifestyle modifications and over-the-counter treatments to medical procedures such as hemorrhoid embolization. You will have the opportunity to ask any questions you may have and discuss any concerns about your symptoms or treatment options. Remember that open communication with your healthcare provider is crucial for effective treatment.
Recovery and Aftercare:
After hemorrhoid embolization, patients usually experience a quick recovery. They can often return to their regular activities within a few days. However, it's important to follow all aftercare instructions provided by the healthcare provider for optimal recovery, including:
Pain Management:
Any post-procedure discomfort can typically be managed with over-the-counter pain relievers. If pain persists or worsens, it's advisable to contact the healthcare provider.
Physical Activity:
Light physical activity, such as walking, can help promote blood flow and expedite healing. However, strenuous activities should be avoided until the healthcare provider gives a go-ahead.
Dietary Adjustments:
Eating a high-fiber diet and drinking plenty of water can help soften stools, reducing the strain on the rectal area and aiding in healing.
Hygiene:
Keeping the anal area clean is crucial to prevent infection. Warm sitz baths may also be recommended to alleviate discomfort and promote healing.
Follow-up Appointments:
Regular follow-up appointments are crucial to monitor the progress of recovery and ensure any complications are addressed promptly.
Medication Adherence:
If the healthcare provider prescribes any medication, such as stool softeners or antibiotics, it's crucial to follow the prescription instructions accurately. This will aid in healing and help prevent complications.